Review Article
Maternal Health Care Service Utilization in Nepal: Trends and Inequalities
1153
Views & Citations153
Likes & Shares
Maternal health is one of the prime concerns for the international community and has prioritized the need to address the reproductive health of woman along with the well-being of the newborn. According to the World Health Organization (WHO), everyday approximately 800 women die from preventable causes related to pregnancy and childbirth. The existence of inequality in health within countries, within different socio-economic and demographic groups, has led to the failure of reaching the target of Millennium Development Goal (MDG) and thus was replaced by Sustainable Development Goal 3. Use of health services is related to the availability, quality and cost of the services that will undoubtedly influence an individual’s decision. Other factors, such as the social structure, health belief, and personal characteristics of the users and the community are also determining factors. There are also several disparities within countries, between women in high and low-income groups and between people living in rural and urban areas. The ladder of progress in maternal health is increasing day by day. Inequality in the utilization of maternal health care by rural-urban places of residence is reducing over time. Special attention needs to be paid to poorer women, those with less education, and those living in remote areas to turn the goals of universal health coverage into reality. In Nepal to increase the utilization of maternal health services, special attention needs to be given to strengthening the health system to raise utilization among poorer women, those with less education, and those living in remote areas.
Keywords: Maternal Health Service Utilization, Factors affecting utilization, Trends, and Inequalities
INTRODUCTION
According to WHO maternal health is define as the health of women during pregnancy, childbirth, and the postpartum period. Maternal health is one of the prime concerns for the international community and has prioritized the need to address the reproductive health of woman along with the well-being of the newborn. Maternal health care is a crucial part of any health care system. According to the World Health Organization (WHO), everyday approximately 800 women die from preventable causes related to pregnancy and childbirth. Out of all maternal deaths, 99 percent occur in developing countries. Further, maternal mortality is higher among women living in rural areas, among poorer communities [1]. Between 2016 and 2030, as part of the Sustainable Development Goals, the target is to reduce the global maternal mortality ratio to less than 70 per 100 000 live births (WHO). In 2015 the maternal mortality ratio in developing countries is 239 per 100 000 live births wherein developed countries it is 12 per 100 000 live births0000. Health care that a woman receives during pregnancy, at the time of childbirth and soon after, is important for the survival and well-being of the mother and the newborn [2]. Various studies conducted in different countries revealed that the utilization of maternal health services is a complex behavioral phenomenon. The use of health services is related to the availability, quality, and cost of the services that will undoubtedly influence an individual’s decision. Other factors, such as the social structure, health belief, and personal characteristics of the users and the community are also determining factors [3-5]. The existence of inequality in health within countries, within different socio-economic and demographic groups, has led to the failure of reaching the target of Millennium Development Goal (MDG) and thus was replaced by Sustainable Development Goal 3 [6]. There are also several disparities within countries, between women in high and low-income groups and between people living in
the rural and urban areas. In developing countries among the adolescent girls under 15 years old the risk of maternal mortality is highest and complications in pregnancy and childbirth is the leading cause of death [7,8]. Among the Dalits, Muslims, and Terai/Madhesi people’s low utilization of maternal health services has been observed. The use of maternal health care is low among those who reside in rural areas and the poor [9,10]. This study aims to identify the trends and inequalities in the utilization of maternal health care services in Nepal.
Lack of awareness about maternal health services
In Nepal especially in rural areas lack of awareness about maternal health has been seen as one of the leading causes of maternal death. Illiteracy and lack of awareness were perceived as major barriers for not utilizing maternal health care services.
One of the participants in the Qualitative study done by Lama and Krishna among pregnant women, postnatal mothers, mothers-in-law, and service providers mentioned, “They do not visit health center because they are not aware of the services and its benefits for our health [11].
Underutilization of maternal health services
In Nepal, the underutilization of health services is a big challenge. In Nepal, different factors hinder service utilization such as lack of awareness, the cost involved in the availability of health facilities, prohibition by the head of the family, less education and low family income are reasons for not delivering children in health institutions [12,13]. Deliveries at home by unskilled birth attendants are still common, in the rural area of Nepal. Women’s low social status, lack of knowledge about illness and lack of awareness about obstetric/gynecological danger signs, lack of decision-making power, and inability to pay for services also play a significant role in the underutilization of existing maternal health service [14].
Factors like: Age, ethnicity, occupation, and education of women as well as their husbands, number of pregnancies and children, use of ANC, and experience of problems during pregnancy are associated with the uptake of skilled delivery care. The main 70 barriers to accessing skilled delivery were distance to hospital and costs associated with delivery at the hospital [15].
Social disparities in maternal health
There was a consistent pattern of disparities in terms of maternal health, among the different groups in the use of ANC, delivery by an SBA, and delivery in a health facility. Less than 35 percent of Muslims, Terai Janajati, and Hill Janajati women received ANC from an SBA; an even lesser percentage delivered in a health facility supported by an SBA. Similarly, Terai / Madhesi Dalits had the lowest percentages delivering in a health facility and has the poorest nutritional status [16].
Unemployment was regarded as an important barrier resulting in a lack of money due to which decision is taken late, and the time is taken to accumulate the assets delays care this was the reason for the women from low economic status for not availing the services. In the Qualitative study done by Lama and Krishna One of the participants mentioned, “Even though the services provided in health centers are free, the cost of transportation and other expenses are high, so people cannot afford to bear the extra costs [11]. Therefore, I think most of the women from remote villages are deprived of services because of a lack of money. The additional costs like transportation cost, investigation costs, and hospital stay expenses cost them higher than the free services provided by health facilities.
Superstition and indigenous practice
In Nepal, still there is the tradition that the first baby should be delivered at home. In some villages of Nepal, a large amount of straw an ideal insulation material is brought into the house to form the birth bed. Women are still forced to give birth in the cowshed. There is some restriction in certain fruits like papaya, pineapple, mango that leads to early labor sometimes leading to abortion. Vitamins are also not given because they believe that vitamins are ‘strengthening’ so it will make the fetus grow big resulting in difficult delivery [11]. These beliefs are the products of social interactions and faith that are entrenched in the minds of the community. Many of these food practices arise due to the ignorance about the nutritive value of food. Most often certain cultural beliefs and practices occurs in the community due to ignorance. One widely held belief is that if a woman eats more during pregnancy, she will have a bigger baby which can cause problems during labor. Studies showed that all these beliefs hurt mothers' and Child’s nutrition and overall health.
Teenage marriage and early pregnancy
Teenage pregnancy still represents one of the most. Important public health problems. Children born by young mothers are at increased risk of sickness and death. Teenage mothers are more likely to experience adverse pregnancy outcomes than young women who delay childbearing. In developing countries, Teenage pregnancies are considered problematic because complications from pregnancy and childbirth are the leading causes of death in teenage girls in developing countries. It is estimated that 70,000 female teenagers die each year because they are pregnant before they are physically mature enough for successful motherhood [17].
METHODOLOGY
Sources of information
EndNote software was used for the literature search and making an electronic library to review the articles concerned with the selected topic. Relevant articles were searched from PUBMED, google scholar, etc. using the relevant terms. The reference lists of key articles were assessed for additional potentially relevant titles. Some of the web-based information was also reviewed and provide some insight regarding the topic.
Search strategy
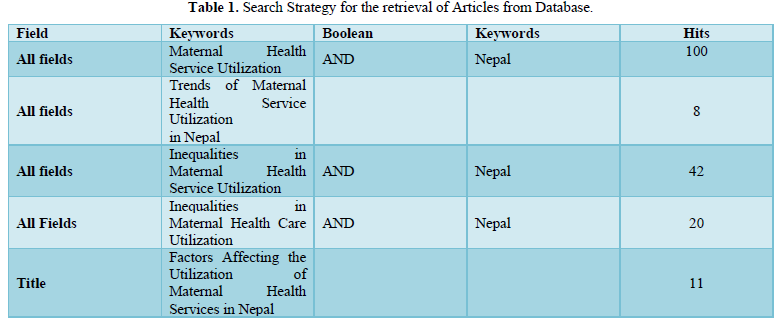
Various terms related to the topic were searched. Various terms used were Maternal Health Service Utilization, Factors affecting utilization, Trends and Inequalities. The results of the Keywords are shown Table 1.
Article selection
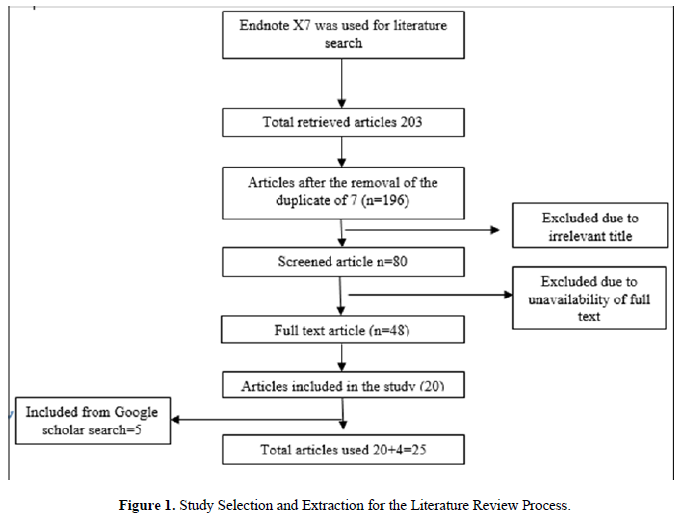
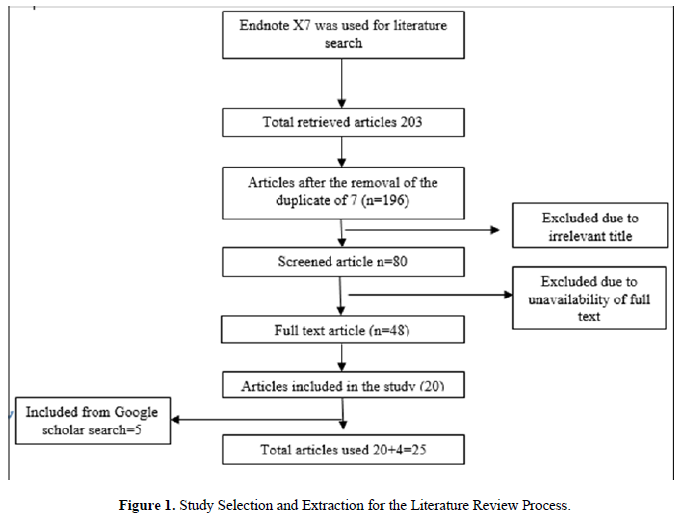
Initially, the search resulted in 181articles from PubMed Endnote x7 and 18 from the google scholar. All together 199 articles were retrieved and after screening for titles and removing irrelevant titled articles is resulted in 80 articles. 48 articles were then assessed for full text only. Finally, articles were included in the review process (Figure 1).
Trends in maternal health care service utilization in Nepal
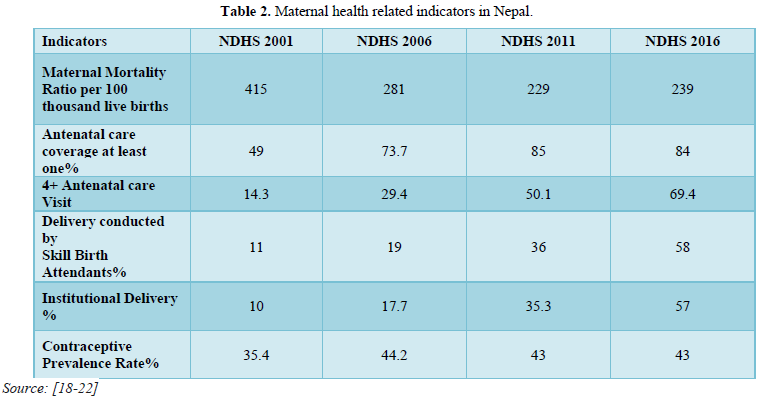
In Nepal maternal health is one of the national priorities and improving maternal health is a major focus of the current national development plan. The trend of maternal death had been significantly reduced by motivating to achieve the target of the Second-Long Term Health Plan i.e., MMR 250 per 100,000 live births by 2017 from 830 per 100,000 live births in 1991 and towards to drop the Millennium Development Goal (MDG 5) target of 134/ 100 thousand live birth by 2015. The ladder of progress in maternal health is increasing day by day. The below table signifies that maternal mortality rate, teenage pregnancy as well as adolescent birth rate have been decreased according to NDHS 2016 in comparison to previous data (Table 2).
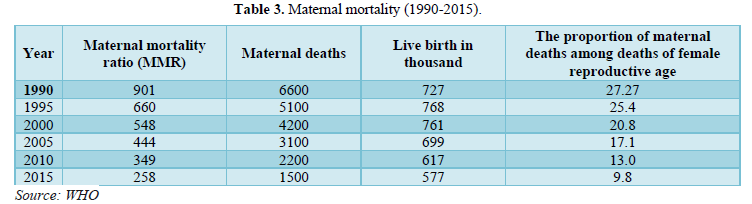
In between the 1996 and 2016 the maternal mortality ratio (MMR) in Nepal decreased from 539 maternal deaths per 100,000 live births to 239 maternal deaths per 100,000 live births. In 2016, 84% of pregnant women had at least one antenatal care (ANC) contact with a skilled provider defined as either a doctor, nurse, or midwife/auxiliary nurse midwife which was a 25% increase from 2011. The percentage of women who had four or more ANC visits increased from 50% in 2011 to 69% in 2016. It was found that the women in the highest wealth quintile with a high education level and those residing in urban areas were much more likely to have four or more ANC from a skilled provider in comparison to the women with lower socioeconomic status and education and those living in rural areas. Between 2011 and 2016, there was a 22% increase in both the proportion of institutional deliveries (from 35% to 57%) and births assisted by SBAs (from 36% to 58%). Doctors assisted 31% of total deliveries, and nurses and midwives/auxiliary nurse midwives assisted 27%. While the percentage of deliveries attended by traditional birth attendants decreased from 11% in 2011 to 5% in 2016, the home birth rate remained high at 41%. Many women in Nepal still deliver with no one present or with an untrained friend or relative (Table 3).
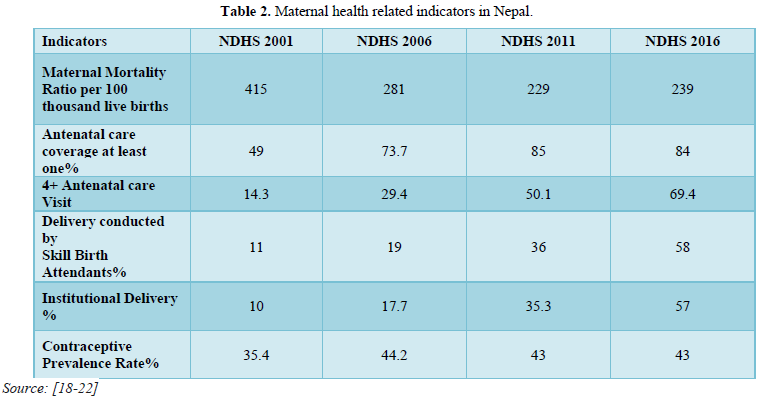
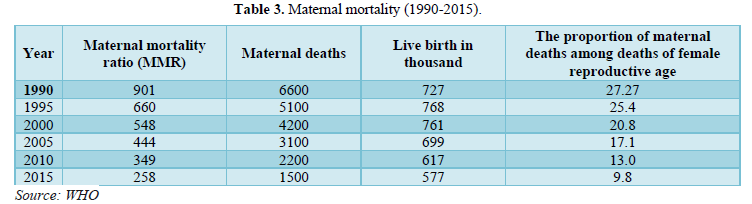
In between the 1996 and 2016 the maternal mortality ratio (MMR) in Nepal decreased from 539 maternal deaths per 100,000 live births to 239 maternal deaths per 100,000 live births. In 2016, 84% of pregnant women had at least one antenatal care (ANC) contact with a skilled provider defined as either a doctor, nurse, or midwife/auxiliary nurse midwife which was a 25% increase from 2011. The percentage of women who had four or more ANC visits increased from 50% in 2011 to 69% in 2016. It was found that the women in the highest wealth quintile with a high education level and those residing in urban areas were much more likely to have four or more ANC from a skilled provider in comparison to the women with lower socioeconomic status and education and those living in rural areas. Between 2011 and 2016, there was a 22% increase in both the proportion of institutional deliveries (from 35% to 57%) and births assisted by SBAs (from 36% to 58%). Doctors assisted 31% of total deliveries, and nurses and midwives/auxiliary nurse midwives assisted 27%. While the percentage of deliveries attended by traditional birth attendants decreased from 11% in 2011 to 5% in 2016, the home birth rate remained high at 41%. Many women in Nepal still deliver with no one present or with an untrained friend or relative (Table 3).
Rural-urban residence
Women from urban areas were nearly 1.5 times more likely to receive four ANC (AOR 1.46; 95% CI: 1.19-1.79), nearly three times more likely to have institutional delivery (AOR 2.72; 95% CI: 2.23-3.31), and nearly twice as likely to deliver by C-section (AOR 1.83; 95% CI: 1.29-2.59) in comparison to women from rural areas. It is important to note that yearly increase for the use of four ANC was 19% in rural areas compared to 12% (95% CI: 8.5%-14.5%) in urban areas.
The yearly increase in institutional delivery rate was 19% (95% CI: 16.3%-20.7%) in rural areas compared to 11% (95% CI: 8.4%-14.6%) in urban areas; and for C-section delivery, the adjusted yearly increase was 14% (95% CI: 9.7%-17.4%) in rural areas and 11% (95% CI: 6.7%-15.7%) in urban areas [20]. Urban women were more likely than rural women to have received ANC from a skilled provider (87% and 80%, respectively) and to have had four or more ANC visits (76% and 62%, respectively). Women in the Hill zone are slightly more likely to receive antenatal care from a skilled provider and to receive more than four ANC visits than women in other zones [22]. Different study data suggest inequality in the use of maternal health care by rural-urban place of residence is reducing over time. A study from India District Level Household and Facility Survey utilization of all selected maternal healthcare services were higher among the urban women compared to the rural women. Only 21 percent of women from the rural area had full ANC as compared to 37 percent of urban women [23].
Caste/ethnicity-based social discrimination
In terms of caste/ethnicity, the highest rate of increase in the use of four ANC was observed among Janajatis (AOR 1.218; 95% CI: 1.182-1.255) and Muslims (AOR: 1.208; 95% CI: 1.133-1.228). For institutional delivery the highest rate of increase was among Janajatis (AOR: 1.190; 95% CI: 1.156-1.226); for C-section, it was for Muslims (AOR: 1.388; 95% CI: 1.169-64.9) [20]. Access to family planning services was lowest among the Dalit and Terai/Madhesi Other, particularly in rural areas, and highest among the Brahman/Chhetri (B/C), Hill Janajatis, and Newars. Similar differences were also noted in access to ANC and the use of SBAs during deliveries; rural Janajati and Dalit women had the least access. There were also social disparities in the nutritional status of mothers and children [10]. A study conducted in India it was found that different forms of discrimination in the sphere of health services against Dalits included separate standing lines, being ignored and kept waiting for long, discrimination in health check-up and treatment, including the avoidance of physical touch, discrimination in the delivery of the medicine and avoidance of visit to houses by public and private doctors and medical practitioners [3]. In a study conducted in India among religious groups, Muslim women had higher utilization of all three maternal healthcare services than the Hindus and women from other religious groups. Around 69% of Muslim women had safe delivery against 51 percent of the Hindus and only 28 percent of women from the other religions [23].
Socioeconomic disparity
In comparison with the C-section and institutional delivery current analysis found inequality in the use of all three maternal health services (4ANC, institutional delivery, and C-section), with inequality greater for C-section delivery than institutional delivery or use of four ANC. Mothers from the richest wealth quintile were more than five times more likely to have 4ANC consultations (AOR: 5.08, 95% CI: 3.82-6.76) [20]. In comparison with the women from the lowest wealth quintile, women from the highest wealth quintile were 9 times more likely to give birth at a facility (AOR 9.00; 95%CI: 6.55-12.37) and nine times more likely to give birth by C-section (AOR 9.37; 95% CI: 4.22-20.83) [20]. According to NDHS 2016, 90% of women in the highest wealth quintile delivered in a health facility, the same was true for only 34% of women in the lowest quintile. 89% of the wealthiest women delivered with an SBA, but only 34% of the poorest women did so. A study conducted in Indonesia it was found that the richest women were 5.45 times (95% CI: 4.75-6.25) more likely to give birth in a health facility and 2.83 times (95% CI: 2.23-3.60) more likely to give birth by C-section than their poorest counterparts [24]. A study conducted in Bangladesh it was found that wealthier and more educated mothers utilized ANC, FBD, and SBA services to a greater extent than socioeconomically disadvantaged women [25]. Socially disadvantaged mothers increased their utilization of care relative to mothers of higher socioeconomic status, the absolute gap in utilization of care between socioeconomic groups has increased over time. District Level Household and Facility Survey conducted in India it was found that the poor women were found to have lower maternal healthcare services utilization than the rich groups. Nearly 14% of the women from the poorest group had full ANC compared to 50% of the women from the richest group. Safe delivery was almost universal among those women from the richest group (92 percent) whereas only 30 percent of the poorest women had safe delivery [23].
Education status
Women who have more education are more likely than those who have less education to receive ANC from a skilled provider. 73% of women with no education received ANC from a skilled provider, compared with 95% of women with an SLC or higher level of education. The proportion of women who receive ANC from a skilled provider increases steadily with wealth. Mothers with higher education were about ten times more likely (AOR: 10.38; 95% CI: 6.81-15.81) to use four ANC compared to women with no education [20]. A study conducted in Ethiopia it was found that the percent of births attended by skilled health personnel in those mothers who were attended secondary schooling & above increased from 45 percent to 74.4 percent between 2000 and 2011. Mothers’ educational status correlates highly with whether their delivery is assisted by a skilled provider and whether the birth is delivered in a health facility. For example, 38% of births to mothers with no education were assisted by a skilled provider, and 36% were delivered in a health facility, as compared with 85% each, of births to mothers with an SLC or higher level of education. A similar relationship is observed with wealth [22].
A study from India it was found that the higher proportions of educated women have used maternal healthcare services than women without any formal education. One of the evidences found that among women with 10 or more years of schooling, 48 percent had received full ANC, 88 percent had safe delivery, and 54 percent had PNC. The corresponding figures among the illiterate women were 13 percent, 28 percent, and 18 percent, respectively [23].
DISCUSSION
Findings from the different studies indicate substantial progress both in increased use and reduced social gradient in the use of these health services. The use of maternal health services in Nepal remains inequitable on many levels. Access to maternal health care especially institutional birth is low in Nepal among women with no or lower education, women from low-wealth quintile households, disadvantaged caste/ethnic groups and women from remote areas. Analysis of data from the four DHS surveys indicates that the most significant determinants of inequality in maternal health use are maternal education and wealth index with both showing an apparent dose-response relationship. From the study, it was found that mothers with higher education were about ten times more likely to used four ANC (AOR: 10.38; 95% CI: 6.81-15.81) compared to women with no education [20]. A study conducted in Ethiopia it was found that the percent of births attended by skilled health personnel in those mothers who were attended secondary schooling & above increased from 45 percent to 74.4 percent between 2000 and 2011.Women from the highest wealth quintile were 9 times more likely to give birth at a health facility (AOR 9.00; 95% CI: 6.55-12.37) and nine times more likely to give birth by C-section (AOR 9.37; 95% CI: 4.22-20.83) in comparison to women from the lowest wealth quintile [20]. A study conducted in Indonesia it was found that the richest women were 5.45 times (95% CI: 4.75-6.25) more likely to give birth in a health facility and 2.83 times (95% CI: 2.23-3.60) more likely to give birth by C-section than their poorest counterparts [24].
CONCLUSION
- The utilization of maternal health services varies according to the socio-economic status of women.
- To turn the goals of universal health coverage into reality, special attention needs to be paid to poorer women, those with less education, and those living in remote areas.
- Higher status women (e.g., measured by education level, wealth, and urban-rural residence) make better use of maternal health services.
- Interventions aim to improve maternal health should be focused on the decision-making power of women their education status and family income.
ACKNOWLEDGEMENT
We would like to thank and acknowledge all the authors and publishers of the reviewed article. We would like to express our thanks to faculty members of the Master of Public Health Program for supporting and providing valuable suggestions.
- World Health Organization (2012) Trends in maternal mortality: 1990 to 2010: WHO, UNICEF, UNFPA and The World Bank estimates. Trends in maternal mortality: 1990 to 2010: WHO, UNICEF, UNFPA and The World Bank estimates. Available online at: http://apps.who.int/iris/bitstream/handle/10665/44874/9789241503631_eng.pdf;jsessionid=B017B14E61A06E0606F3E6AB894F7A4C?sequence=1
- Shrestha G (2017) Factors Affecting Maternal Health Care Services Utilization in Nepal: Insight from the Nepal Demographic Health Survey 2006 and 2011. Nep J Stat 1: 55-72.
- George S (2015) Caste and Care: Is Indian Healthcare Delivery System Favorable for Dalits: Institute for Social and Economic Change. Available online at: http://www.isec.ac.in/WP%20350%20-%20Sobin%20George.pdf
- Becker S, Peters DH, Gray RH, Gultiano C, Black RE (1993) The determinants of use of maternal and child health services in Metro Cebu, the Philippines. Health Transit Rev 3(1): 77-89.
- Andersen RM (1995) Revisiting the behavioral model and access to medical care: Does it matter? J Health Social Behav 36(1): 1-10.
- Yadav P, Yadav AK (2017) Out-of-Pocket Expenditure in Maternal Health Care in High-Focus States of India. Demography India. pp: 143-152. Available online at: http://demographyindia.in/article_document/48/1318016.pdf
- Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, et al. (2009) Global patterns of mortality in young people: a systematic analysis of population health data. Lancet 374(9693): 881-892.
- Conde-Agudelo A, Belizán JM, Lammers C (2005) Maternal-perinatal morbidity and mortality associated with adolescent pregnancy in Latin America: Cross-sectional study. Am J Obstet Gynecol 192(2): 342-349.
- Mehata S, Baral S, Chand P, Singh D, Poudel P et al. (2013) Nepal Household Survey. Ministry of Health and Population (MOHP), Government of Nepal, Kathmandu, Nepal. Available online at: https://www.mohp.gov.np/downloads/Household%20Survey%202012.pdf
- Kathmandu N (2013) Maternal and child health in Nepal: The effects of caste, ethnicity, and regional identity. Available online at: https://www.dhsprogram.com/pubs/pdf/FA73/FA73.pdf
- Lama S, Krishna AKI (2014) Barriers in utilization of maternal health care services: Perceptions of rural women in Eastern Nepal. Kathmandu Univ Med J (KUMJ) 12(4): 253-258.
- Simkhada B, Van Teijlingen E, Porter M, Simkhada P (2006) Major problems and key issues in Maternal Health in Nepal. Kathmandu Univ Med J (KUMJ) 4(2): 258-63.
- Pokhrel B, Sharma P, Bhatta B, Bhandari B, Jha N (2012) Health seeking behavior during pregnancy and child birth among Muslim women of Biratnager, Nepal. Nepal Med Coll J 14(2): 125-128.
- Baral YR, Lyons K, Skinner J, Van TER (2012) Maternal health services utilization in Nepal: Progress in the new millennium? Health Sci J 6(4): 618.
- Dhakal S, Van TER, Raja EA, Dhakal KB (2011) Skilled care at birth among rural women in Nepal: Practice and challenges. J Health Popul Nutr 29(4): 371.
- Bennett L, Dahal DR, Govindasamy P (2008) Caste, ethnic, and regional identity in Nepal: further analysis of the 2006 Nepal Demographic and Health Survey: Population Division, Ministry of Health and Population, Government of Nepal. Available online at: https://dhsprogram.com/pubs/pdf/FA58/FA58.pdf
- Mayor S (2004) Pregnancy and childbirth are leading causes of death in teenage girls in developing countries. BMJ 328(7449): 1152.
- Nepal Demographic and Health Survey (2006) Available online at: https://dhsprogram.com/pubs/pdf/FR191/FR191.pdf
- Nepal Demographic and Health Survey (2011) Available online at: https://dhsprogram.com/pubs/pdf/fr257/fr257%5B13april2012%5D.pdf
- Mehata S, Paudel YR, Dariang M, Aryal KK, Lal BK et al. (2017) Trends and inequalities in use of maternal health care services in Nepal: Strategy in the search for improvements. BioMed Res Int 2017: 1-11
- Demographic and Health Survey (2001) Available online at: https://microdata.worldbank.org/index.php/catalog/1464
- Nepal Demographic and Health Survey (2016) Available online at: https://www.dhsprogram.com/pubs/pdf/fr336/fr336.pdf
- Prusty RK, Gouda J, Pradhan MR (2015) Inequality in the utilization of maternal healthcare services in Odisha, India. Int J Popul Res 2015: 1-10.
- Nababan HY, Hasan M, Marthias T, Dhital R, Rahman A, et al. (2018) Trends and inequities in use of maternal health care services in Indonesia, 1986-2012. Int J Womens Health 10: 11-24.
- Hajizadeh M, Alam N, Nandi A (2014) Social inequalities in the utilization of maternal care in Bangladesh: Have they widened or narrowed in recent years? Int J Equity Health 13(1): 120.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Allergy Research (ISSN:2642-326X)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)


